-
Venous Disease/Chronic Venous Insufficiency
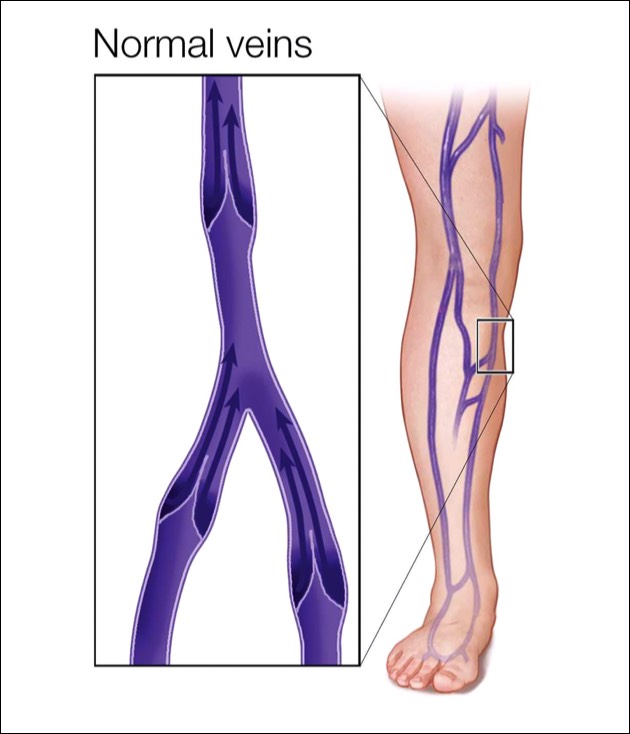
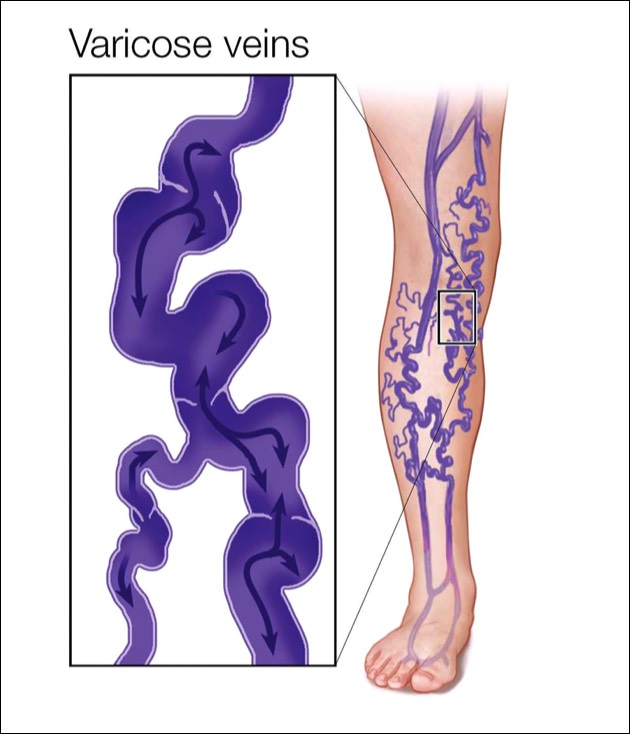
Your veins are vessels that carry blood from your body's tissues to your heart and lungs to pick up more oxygen and get re-circulated through your body. The muscles in your legs aid in this process, contracting to help pump the blood upward. Veins have tiny valves inside them to keep the blood flowing in the right direction; this one-way traffic keeps blood from flowing backward. However, a malfunction can occur in one or more of these valves, a common condition we call venous insufficiency. Venous insufficiency is what causes varicose veins and spider veins and affects more than 30 million Americans.
Varicose veins are swollen and often visible, twisted, blue or colorless veins that are close to the surface of the skin and often appear as bulges. Because valves in these veins are damaged, they hold more blood at higher pressure than normal.
Legs With Varicose Veins
Legs With Varicose Veins
Normal Veins, Healthy Valves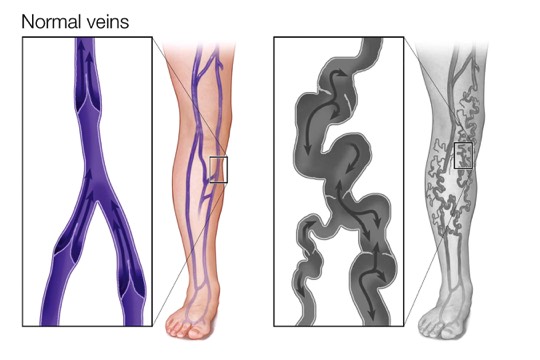
Normal Veins, Healthy Valves
Unhealthy Veins, Damaged Valves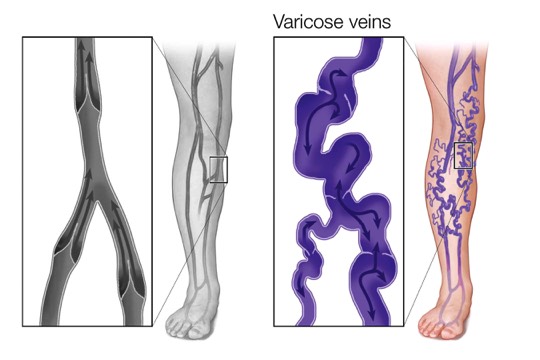
Unhealthy Veins, Damaged Valves
-
What are the Symptoms?
Varicose Veins may be asymptomatic. Some symptoms may include:
Pain, itching, swelling, burning, leg heaviness or tiredness, skin discoloration. Symptoms typically worsen throughout the day and are partially relieved by elevation or wearing compression socks or stockings.
Sometimes, varicose veins clot and become painful, hot, hard and discolored. This is called phlebitis, an uncomfortable but temporary condition that will get better on its own in 2-3 months. Clots associated with phlebitis are limited to surface veins, and are not dangerous, unlike clots in the deep veins (deep vein thrombosis or DVT) that are dangerous because they can travel to the heart or lung and require prompt treatment with blood thinners.
A shower or minor trauma can cause a varicose vein to burst and bleed, also skin tears or ulcerations indicate a very severe case. -
What are the Risk Factors?
Varicose veins affect up to 35% of people in the United States.
Women are more likely to develop varicose veins. Hormonal changes during pregnancy, pre-menstruation or menopause may be a factor because female hormones tend to relax vein walls. Varicose veins that develop during pregnancy generally improve without medical treatment 3 to 12 months after delivery. Taking hormone replacement therapy or birth control pills may increase your risk of varicose veins.
Family history is another factor. If other family members have had varicose veins, there's a greater chance you will too.
Obesity or being overweight puts added pressure on your veins.
Standing or sitting for long periods of time may be another risk factor. -
How is the Diagnosis Made?
To diagnose varicose veins, your doctor will do a physical exam, including looking at your legs while you're standing to check for swelling. Your doctor may also ask you to describe any pain and aching in your legs. You may also need an ultrasound test to see if the valves in your veins are functioning normally or if there's any evidence of a blood clot, and to rule out more serious problems. Your evaluation will determine the causes and extent of the problem.
What is Ultrasound?Ultrasound is a non-invasive test that looks at the blood flowing through your veins. Advanced imaging machines using ultrasound can painlessly, and non-invasively produce pictures showing the blood vessels and the blood flowing through them. A small transducer is pressed against the skin utilizing sound waves to create images in your legs to a monitor, so a technician and your doctor can see them. The test can show changes in blood flow due to narrowing or blockage, which help the doctor rule out more serious vein conditions.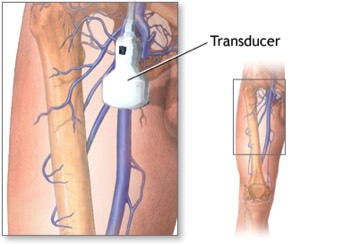
-
Treatment
After your evaluation, you will work with your doctor to develop a treatment plan. Your treatment plan may include, compression stockings, injections, minimally invasive procedures, and surgery. Fortunately, treatment doesn't mean a hospital stay or a long uncomfortable recovery. Thanks to less invasive procedures, varicose veins can generally be treated on an outpatient basis.
Ask your doctor if insurance will cover any of the cost of your treatment. If done for purely cosmetic reasons, you'll likely have to pay for the treatment of varicose veins.-
Compression Stockings

Wearing compression stockings all day is often the first approach to try before moving on to other treatments. They steadily squeeze your legs, helping veins and leg muscles move blood more efficiently. The amount of compression varies by type and brand. You can buy compression stockings at most pharmacies and medical supply stores. Check with your doctor before buying compression stockings, so you can get the correct pressure and size.Tips for Using Compression Stockings
- Make sure to wear them correctly. Pull them to the designated height and no further. Don’t let them bunch up at the top, as this can restrict circulation.
- Replace them when they start to become loose, which is often after about 4 to 6 months.
- Don’t sleep in them unless so directed.
- Wear the length recommended by your doctor.
- Wear them as recommended by your doctor.
- If you have trouble pulling them on, wear thin rubber gloves to help improve your grip and prevent tearing. You can also use equipment, such as a stocking donner, to help put them on.
-
Endovenous Ablation
Endovenous ablation treats varicose veins in the superficial venous system. The procedure is performed on an outpatient basis, under conscious sedation. Using ultrasound, your surgeon will guide a catheter into the diseased vein through a micro incision made in the skin. Radiofrequency delivers heat to the vein wall through the catheter. As the thermal energy is delivered, the vein wall shrinks, and the vein is sealed closed. This causes the blood to re-route to other healthy veins.
Following the procedure, a small bandage is placed over the insertion site and additional compression may be provided to aid healing. The average patient typically resumes normal activity within a few days.
Interview with SFVVG's Dr. Nassoura on the diagnosis and treatment of varicose veins. -
Varithena
Varithena treatment is a minimally invasive procedure which involves injecting foam into diseased veins to close them down allowing blood to flow to other healthier veins. With Varithena there are no incisions, sedation or general anesthesia. The procedure can usually be completed in less than an hour, and most people only need a single treatment to see results. Varithena dissolves in the bloodstream after treatment leaving nothing permanently in your vein.Varithena
-
VenaSeal
The VenaSeal system improves blood flow by sealing or closing the diseased vein. The system delivers a small amount of a specially formulated medical adhesive to the diseased vein. The adhesive seals the vein and blood is rerouted through nearby healthy veins.VenaSeal
-
Excision (Phlebectomy)
Excision is a technique used to remove varicose veins.
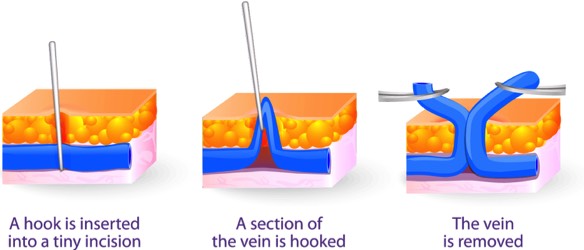
Several tiny cuts are made in the skin, through which the varicosed vein is removed.
Excision may be used along with other treatments and is performed on an out-patient basis.
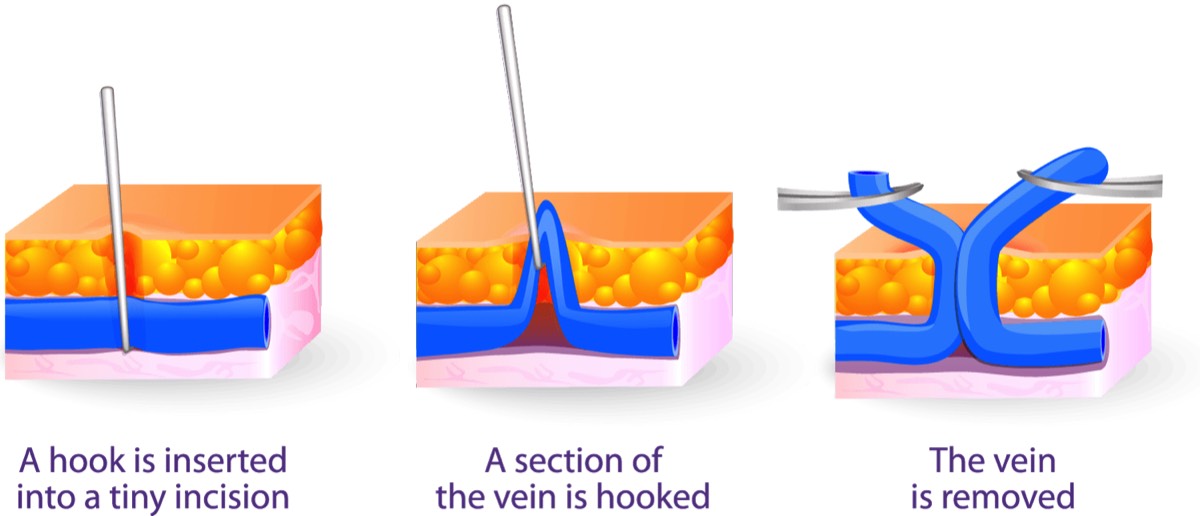
Excision is a technique used to remove varicose veins.
Several tiny cuts are made in the skin, through which the varicosed vein is removed.
Excision is performed on an out-patient basis.
-
Compression Stockings
-
Self-Care
There are certain things you can do on your own to try to ease pain and prevent varicose veins from getting worse, such as:
- Exercise
- Lose weight
- Don’t wear tight fitting clothing
- Elevate your legs
- Avoid standing or sitting for long periods of time.
ExerciseWorking calf and thigh muscles helps move blood upward. Keeping these muscles toned may help with blood flow even when you’re sitting or standing.
To get the most benefit:
- Choose exercise that work the leg muscles. Walking, swimming, and cycling, are great choices.
- If you’re new to exercise, start slowly and build up to at least 30 minutes of exercise most days of the week.
- If you sit most of the day, get up and walk from time to time. Just changing position may offer some relief. Also try wiggling your toes for a minute 10 times a day.
ElevationRaising your legs lets gravity help blood flow back to the heart. For the most benefit, raise your feet a few inches above your heart, 2 to 3 times a day for 15 minutes, if possible. Any elevation will help. -
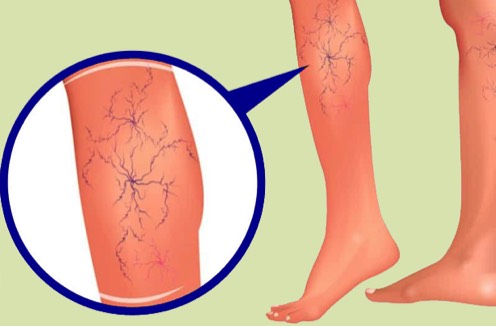
What are Spider Veins?
Spider veins are not true varicose veins, but rather they are tangled groups of tiny blood vessels just under the skin surface that resemble spider webs or tree branches. Typically, they are red, blue or purple and are clearly visible on the thighs and lower legs. Spider veins are usually harmless, though they can sometimes cause an aching, burning or pain, especially when you've been standing for long periods. People with a family history of varicose veins or spider veins have the highest risk of developing them. In fact, even athletes and young women and men can develop varicose veins if they have a family history of venous insufficiency.
-
Treatment
Our doctor will perform an evaluation to ensure that there isn't an underlying component that's causing your spider veins. If he discovers an underlying issue, the issue must be treated first before treating the spider veins to ensure that your spider veins will resolve. If he determines that no other issues exist, then your spider veins will typically be treated with a combination of sclerotherapy and laser therapy.
-
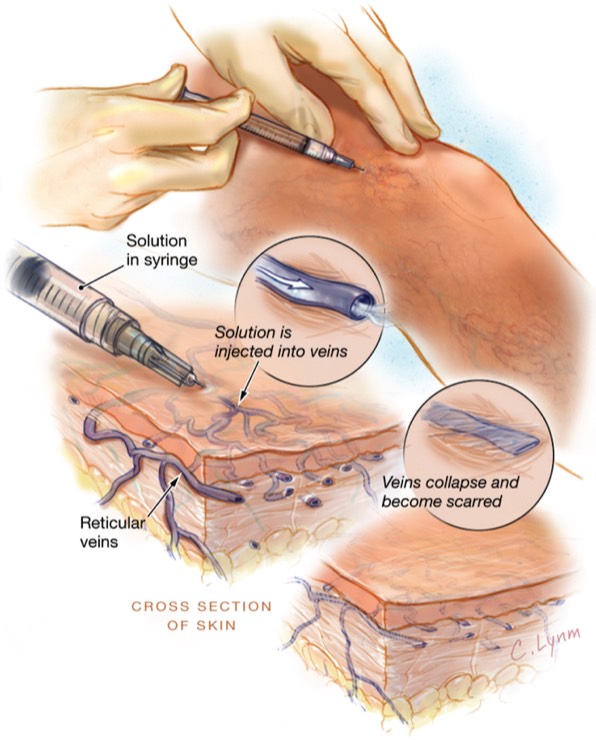
What is Sclerotherapy?
Sclerotherapy is a medical procedure that does not require anesthesia and is performed on an out-patient basis in our office. Sclerotherapy is used to eliminate small varicose veins and spider veins.
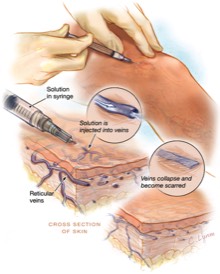
In this procedure, your doctor injects small and medium sized varicose veins with a solution that scars and closes those veins. In a few weeks, treated veins should fade.
Although the same vein may need to be injected more than once, sclerotherapy is effective when done correctly.
Compression stockings are required to be worn for three days after the procedure.
Sclerotherapy, unfortunately, is not covered by insurance.
-
What is Laser?
Laser treatments use a powerful, focused light beam to heat the inside of the vessel. The laser light bypasses the outer layer of the skin, sending strong bursts of light onto the vein, which injures the small blood vessels of the leg. This causes them to gradually shrink and disappear. This treatment works best for small to medium sized vessels. 1 to 3 sessions may be required. This procedure is not covered by insurance.

Compression stockings are required to be worn for three days after the procedure.
-
What is Sclerotherapy?