-
Abdominal Aortic Aneurysm
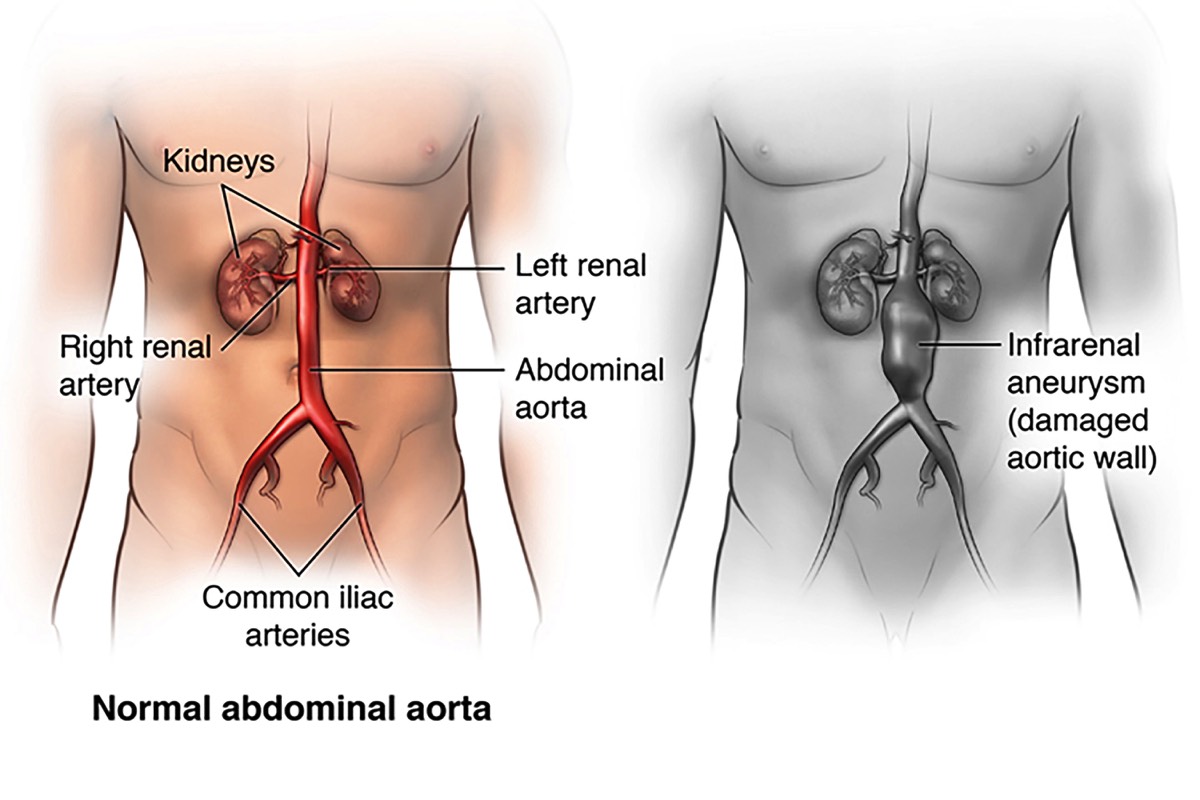
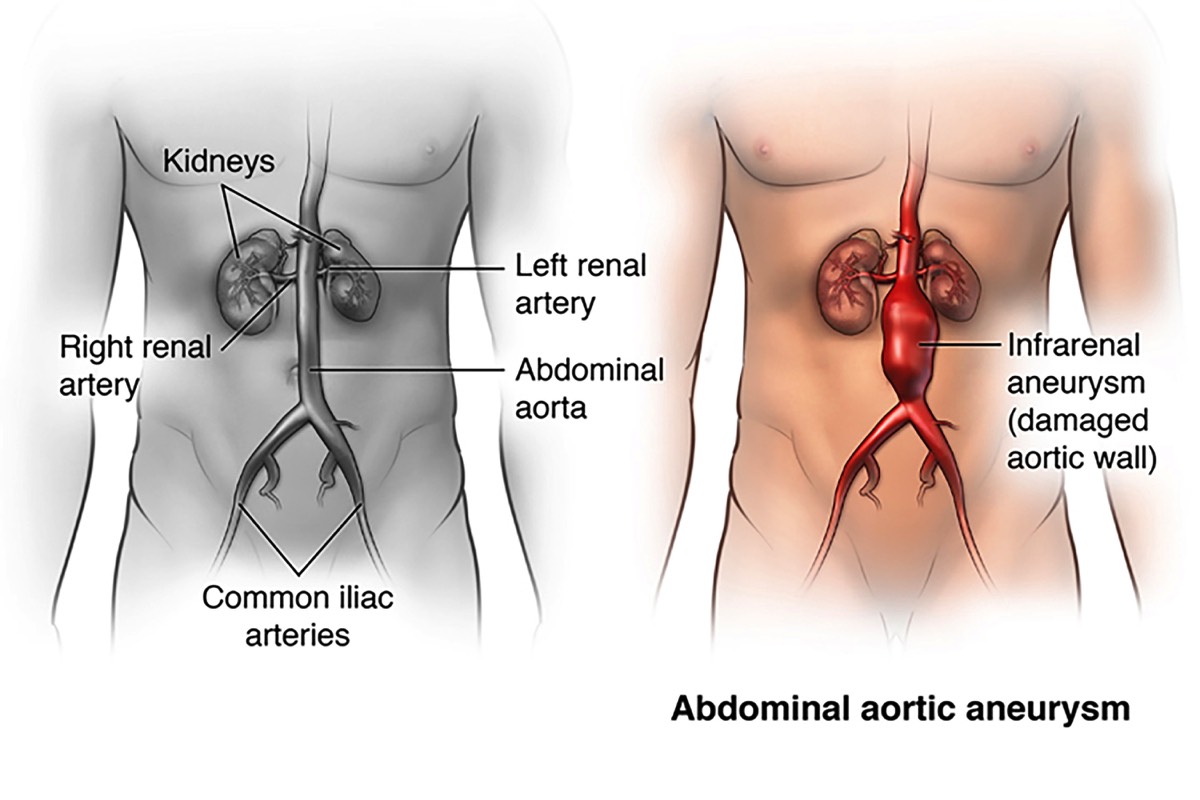
The aorta is the largest artery in your body, and it carries oxygen-rich blood pumped out of, or away from your heart. Your aorta runs through your chest, where it is called the thoracic aorta. Once it reaches your abdomen, it is called the abdominal aorta. The abdominal aorta supplies blood to the lower part of the body. In the abdomen, just below the navel, the aorta splits into two branches, called the iliac arteries, which carry blood to each leg.
An abdominal aortic aneurysm, or AAA, is a balloon-like bulge in the abdominal aorta. The bulge forms a weak spot in the wall of the aorta. The pressure generated by each heartbeat, pushes against the weakened aortic wall, causing the aneurysm to enlarge. Ultimately, the aneurysm becomes so large, and its wall so weak, that rupture occurs. This can be fatal, due to massive bleeding.
Fortunately, especially when diagnosed early before it causes symptoms, or rupture, an AAA can be treated, or even cured, with highly effective and safe treatments.
Healthy Abdominal AortaHealthy Abdominal Aorta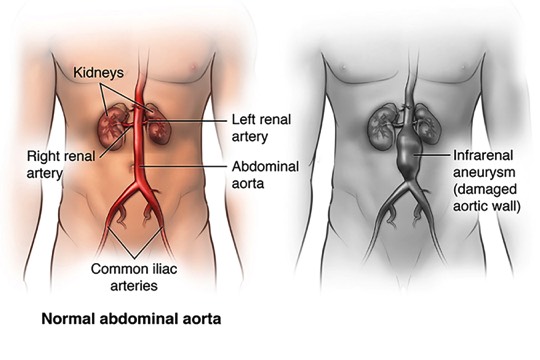 The abdominal aorta carries oxygen-rich blood from the heart to the lower body.Weakened Aorta WallWeakened Aorta Wall
The abdominal aorta carries oxygen-rich blood from the heart to the lower body.Weakened Aorta WallWeakened Aorta Wall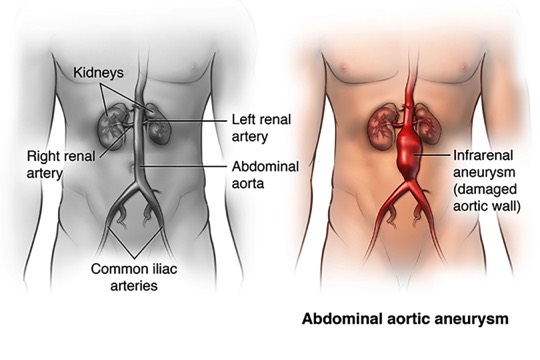 An aneurysm forms when part of the wall of the aorta weakens and balloons outward.Plaque in Artery WallPlaque in Artery Wall
An aneurysm forms when part of the wall of the aorta weakens and balloons outward.Plaque in Artery WallPlaque in Artery Wall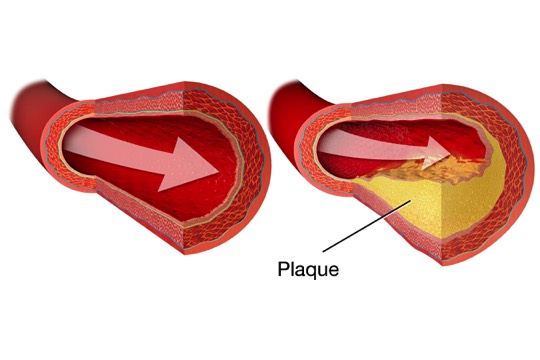 Plaque may be found in the weakened artery wall. Blood may thicken (clot) inside the artery. Blood can still flow through the clot, so this may not cause symptoms.
Plaque may be found in the weakened artery wall. Blood may thicken (clot) inside the artery. Blood can still flow through the clot, so this may not cause symptoms. -
What are the Symptoms?
An AAA is called a “silent” problem, because it usually causes no symptoms. It’s sometimes found by a healthcare provider during a routine exam. More often, it’s detected when tests are being performed for an unrelated issue (x-ray, ultrasound, CT scan, MRI). Once an AAA has been found, tests will be done to measure its size and follow its growth. Symptoms include one or more of the following:
- A pulsing feeling in your abdomen, similar to a heartbeat
- Severe, sudden pain in your abdomen or lower back. If this is the case, your aneurysm may be about to burst
- On rare occasions, your feet may develop pain, discoloration, or sores on the toes or feet because of material shed from the aneurysm
If your aneurysm bursts, you may suddenly experience intense weakness, dizziness, or pain, and you may eventually lose consciousness.
This is a life-threatening situation and you should seek medical attention immediately. -
What are the Risk Factors?
Anyone can have an AAA. But certain factors increase the risk that an AAA will rupture. AAA is more common in men than women. The risk of developing and abdominal aneurysm increases as you age. Other factors that increase your risk of AAA include:
- Smoking
- Family history - Immediate relative such as a mother or father or siblings, who have had an AAA
- High blood pressure
- High cholesterol
- Having blood vessel disease in another part of your body
- Being over 60 if you’re a man, or over age 65 if you’re a woman
- Emphysema
-
How is the Diagnosis Made?
Your doctor will perform a physical exam, which may include an exam of your abdomen. He will ask about your health history and your family health history. He will do an abdominal ultrasound, and may order other imaging tests, such as a CT scan.
What is a Ultrasonography?Ultrasonography is a non-invasive test which must be performed FASTING on an EMPTY STOMACH (at least 8 hours prior to the procedure). A small transducer is pressed against your abdomen, utilizing sound waves to create an image of the blood vessels. For this test, gel is applied to your abdomen as it helps the scanner collect sound waves while it’s moved across your abdomen. It will identify an aneurysm if present, and determines its size.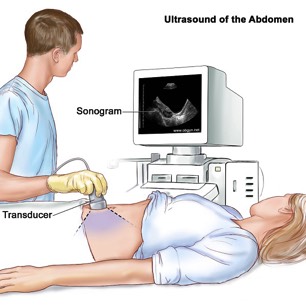
What is a CT Scan?The CT scan is the ultimate test prior to planning surgical repair. A CT (computed tomography) is a series of x-rays taken with a special machine. Computers use these x-rays to create three-dimensional images. CT angiography (CTA) requires injection of contrast fluid (dye) through an IV line, to make blood vessels visible on the x-ray image. This helps arteries show up clearly.
Inform your doctor if you are allergic to the contrast fluid (dye) given during CT scan. -
Treatment
An AAA can be repaired using endovascular repair or open surgery. Both methods involve placing an artificial graft inside the damaged artery. Your options for treatment depend on many factors that your physician will discuss with you, such as, how big your aneurysm is, is it growing, and if so, how quickly? Your overall health is also a consideration. If your aneurysm is small, your doctor may also suggest “watchful waiting".
You and your doctor will discuss and weigh the benefits and risks of each type of treatment, and a decision will be made about how to proceed.
What is "Watchful Waiting"?If your aneurysm is small, your physician may recommend “watching waiting”, which means that you will be monitored every 6-12 months for signs of changes in the aneurysm size. It also means being alert for symptoms of rupture, such as severe back pain, tenderness in your abdominal area, or lightheadedness or the feeling of dizziness. Call 911 right away, if you experience these symptoms.
Your physician may schedule you for regular CT scans or ultrasounds to watch the aneurysm. This method is usually used for aneurysms that are smaller than about 2 inches (roughly 5.0 to 5.5 centimeters) in diameter.
If you smoke, you should seek help to quit smoking. An aneurysm will not “go away” by itself. It is extremely important to continue to follow up with your physician as directed because the aneurysm may enlarge to a dangerous size over time. It could eventually burst if this is not detected and treated.
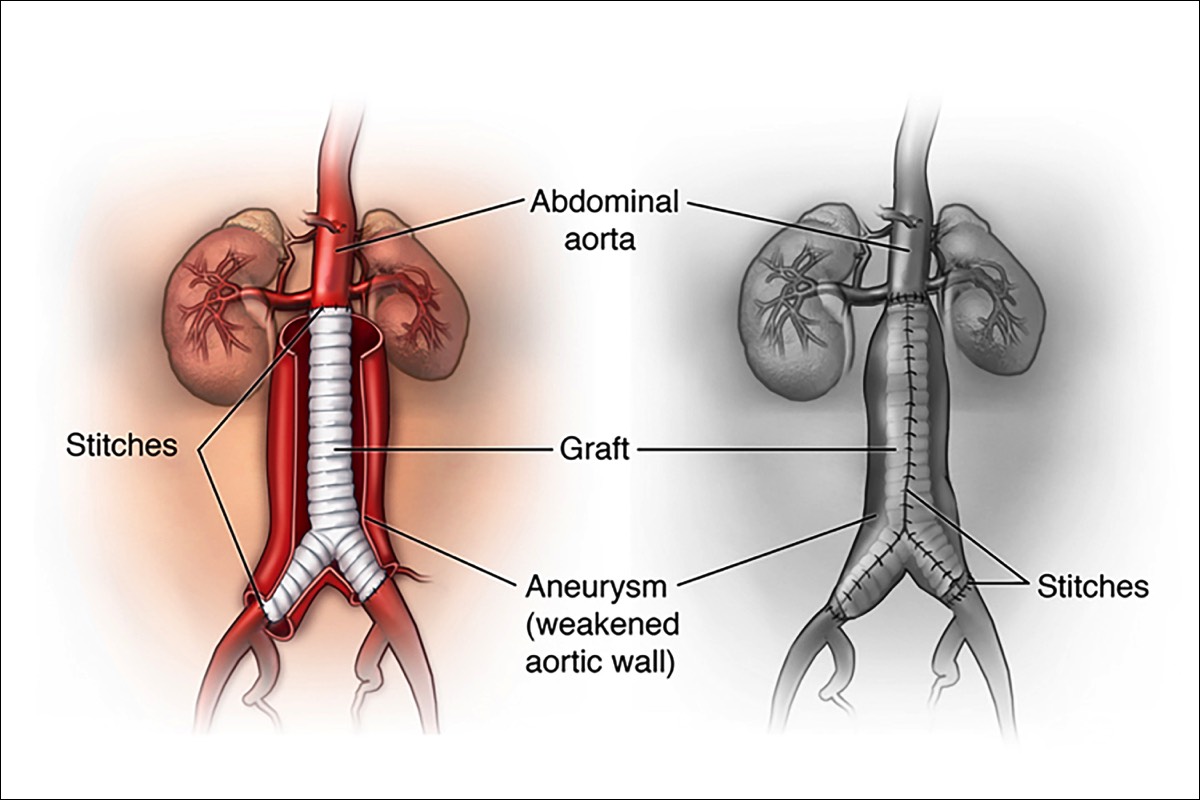
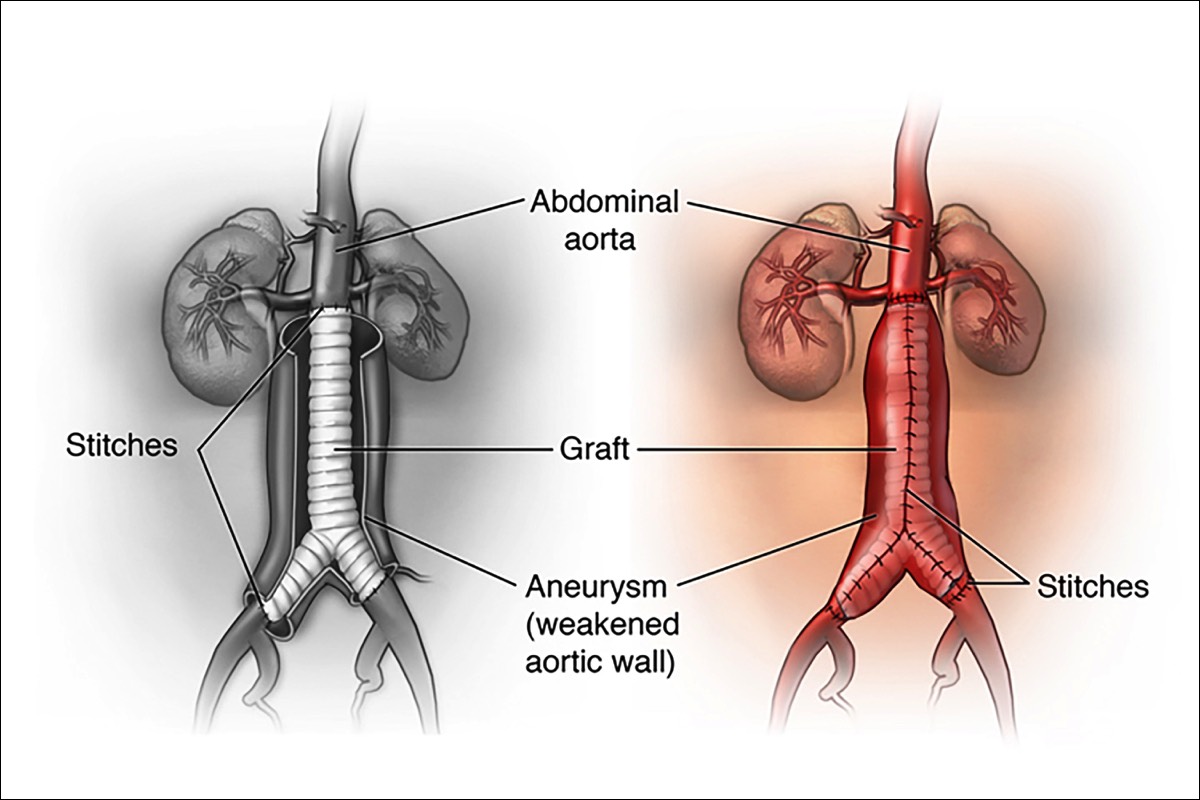
What is Open Surgical Aneurysm Repair?An open aneurysm repair, is also known as surgical aneurysm repair. During an open aneurysm repair, your surgeon makes an incision in your abdomen and replaces the weakened part of your aorta with a tube-like replacement called an aortic graft. This graft is made of a strong, durable, man-made plastic material, such as Dacron, in the size and shape of the healthy aorta. The strong tube takes the place of the weakened section in your aorta and allows your blood to pass easily through it. Following the surgery, you may stay in the hospital for 5 to 7 days. Depending upon your circumstances, you may also require 6 weeks to 3 months for a complete recovery. More than 90% of open aneurysm repairs are successful for the long term.Surgery Step 1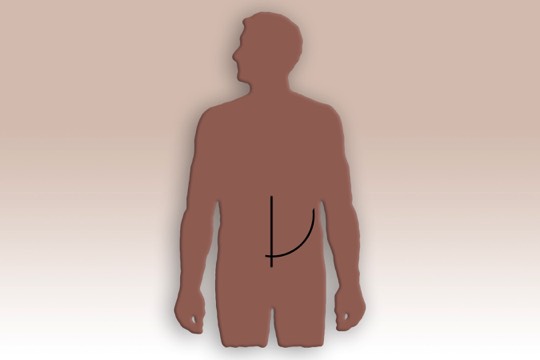 Surgery begins with an incision in your abdomen. Two possible positions for this incision are shown in this example. The one shown here as a curve, may continue around the side of the body. The size and shape of your own incision may vary.Surgery Step 2
Surgery begins with an incision in your abdomen. Two possible positions for this incision are shown in this example. The one shown here as a curve, may continue around the side of the body. The size and shape of your own incision may vary.Surgery Step 2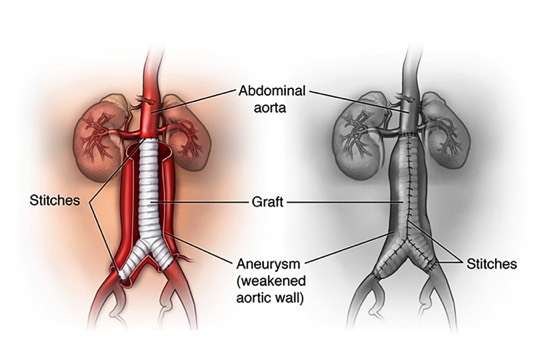 The surgeon moves aside the organs to reach the aorta. The aorta is clamped to stop blood flow. The surgeon then opens the aneurysm and clears any blood clot. The graft is sewn to the aorta above and below the aneurysm.Surgery Step 3
The surgeon moves aside the organs to reach the aorta. The aorta is clamped to stop blood flow. The surgeon then opens the aneurysm and clears any blood clot. The graft is sewn to the aorta above and below the aneurysm.Surgery Step 3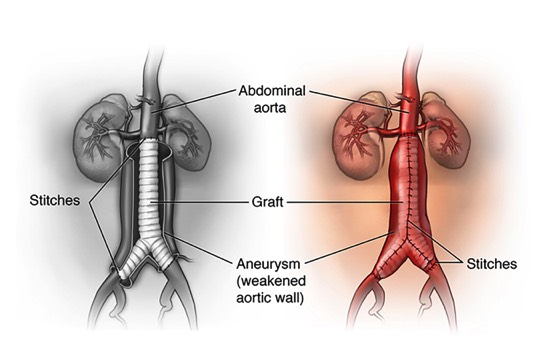 Some of the aorta wall may be removed. This helps make a snug fit when the aorta is wrapped around the graft. The aorta is then sewn together, helping to protect the graft. The incision site is closed.
Some of the aorta wall may be removed. This helps make a snug fit when the aorta is wrapped around the graft. The aorta is then sewn together, helping to protect the graft. The incision site is closed.
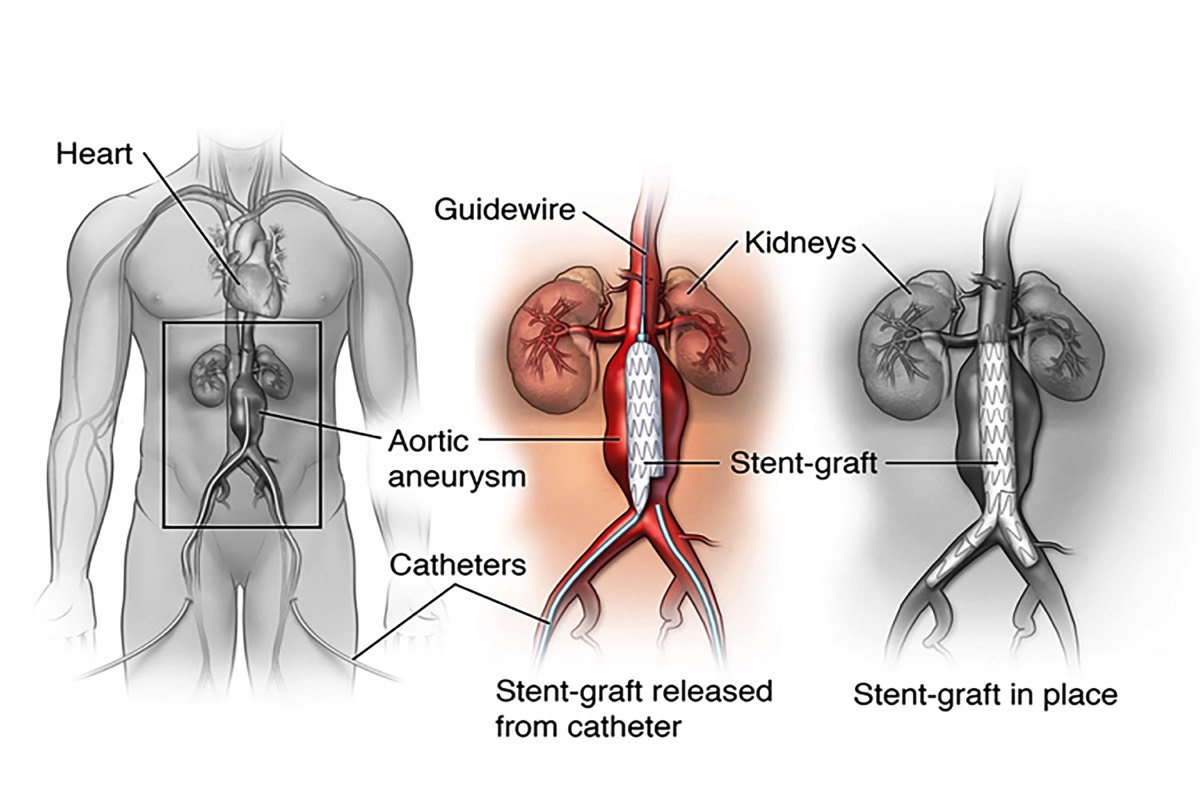
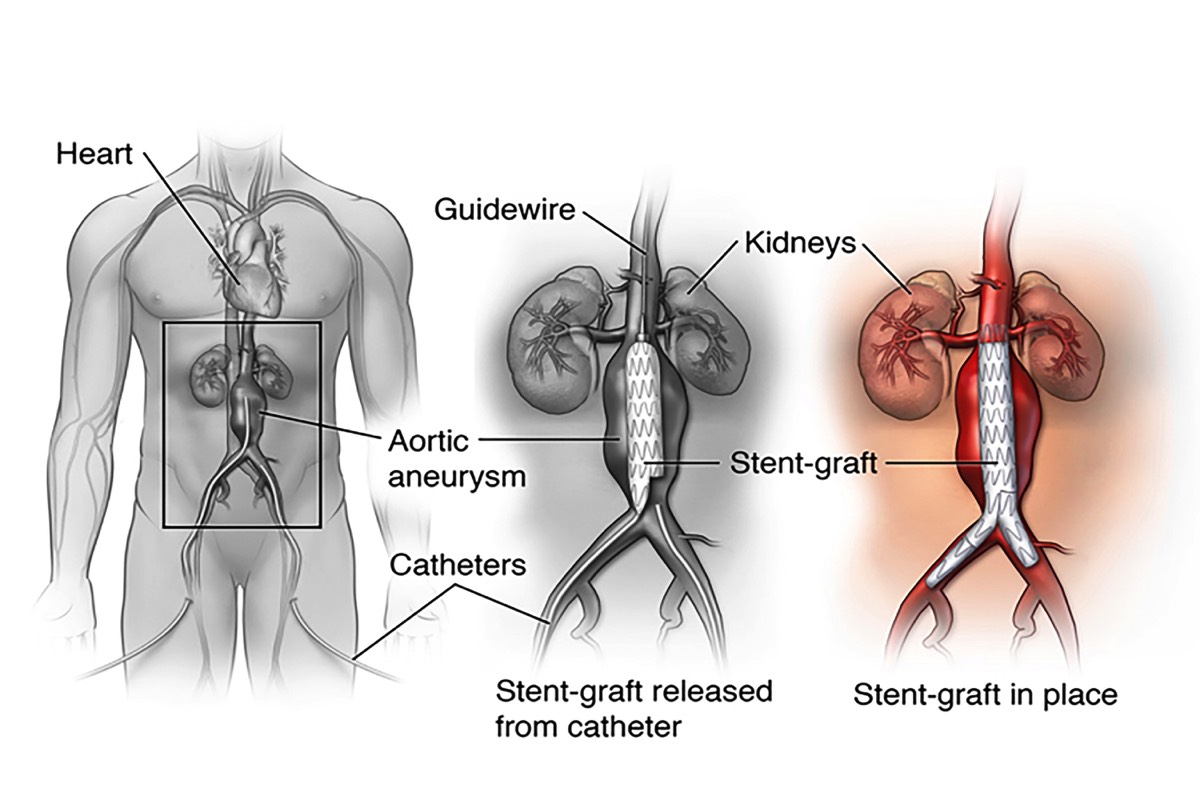
What is Endovascular Aneurysm Repair (EVAR)?Endovascular repair is performed inside your artery using long, thin tubes called catheters that are threaded through your blood vessels. This procedure is less invasive, meaning that your surgeon will usually need to only make small incisions in your groin area through which to thread the catheters. During the procedure, your surgeon will use live x-ray pictures viewed on a video screen to guide a fabric and metal tube, called an endovascular stent graft, (or endograft) to the site of the aneurysm. Like the graft in open surgery, the endovascular stent graft also strengthens the aorta. Your recovery time for endovascular stent grafting is usually shorter than for the open surgery, and your hospital stay may be reduced to 1-2 days. However, this procedure requires yearly follow-up visits with imaging procedures, usually CT scan, after endograft placement to be sure the graft continues to function properly.Surgery Step 1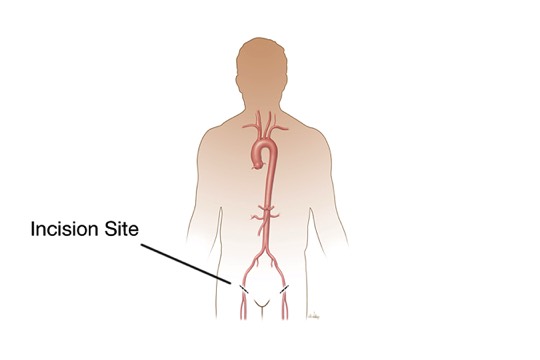 Two small incisions are made in the groin. A catheter (thin, flexible tube) is threaded through an artery at each incision. The collapsed graft is placed inside one of the catheters.Surgery Step 2
Two small incisions are made in the groin. A catheter (thin, flexible tube) is threaded through an artery at each incision. The collapsed graft is placed inside one of the catheters.Surgery Step 2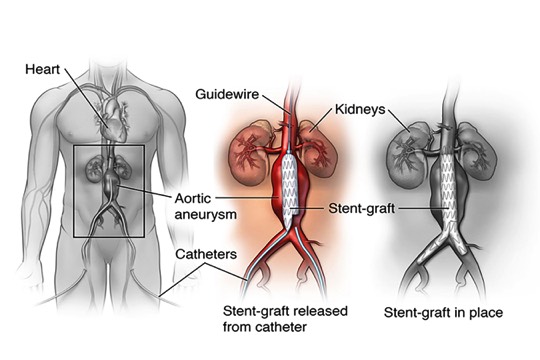 The surgeon uses x-ray guidance to move the graft through the arteries toward the damaged part of the aorta. The catheters are then used to place the graft in position.Surgery Step 3
The surgeon uses x-ray guidance to move the graft through the arteries toward the damaged part of the aorta. The catheters are then used to place the graft in position.Surgery Step 3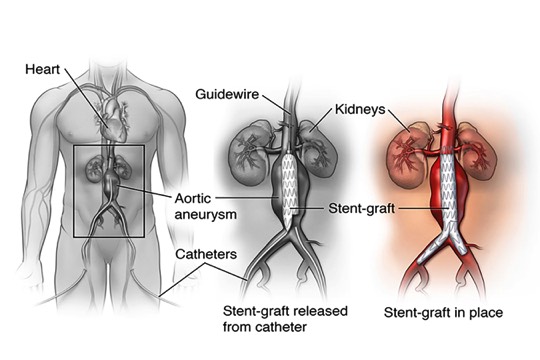 Once the graft is in position, the surgeon expands it. Metal springs or hooks hold it in place above and below the aneurysm. The catheters are then removed.
Once the graft is in position, the surgeon expands it. Metal springs or hooks hold it in place above and below the aneurysm. The catheters are then removed.
Open and Endovascular Abdominal Aortic Aneurysm
Fenestrated Endovascular Aneurysm Repair“Permission for use granted by Cook Medical Incorporated, Bloomington, Indiana”