-
Thoracic Aortic Aneurysm
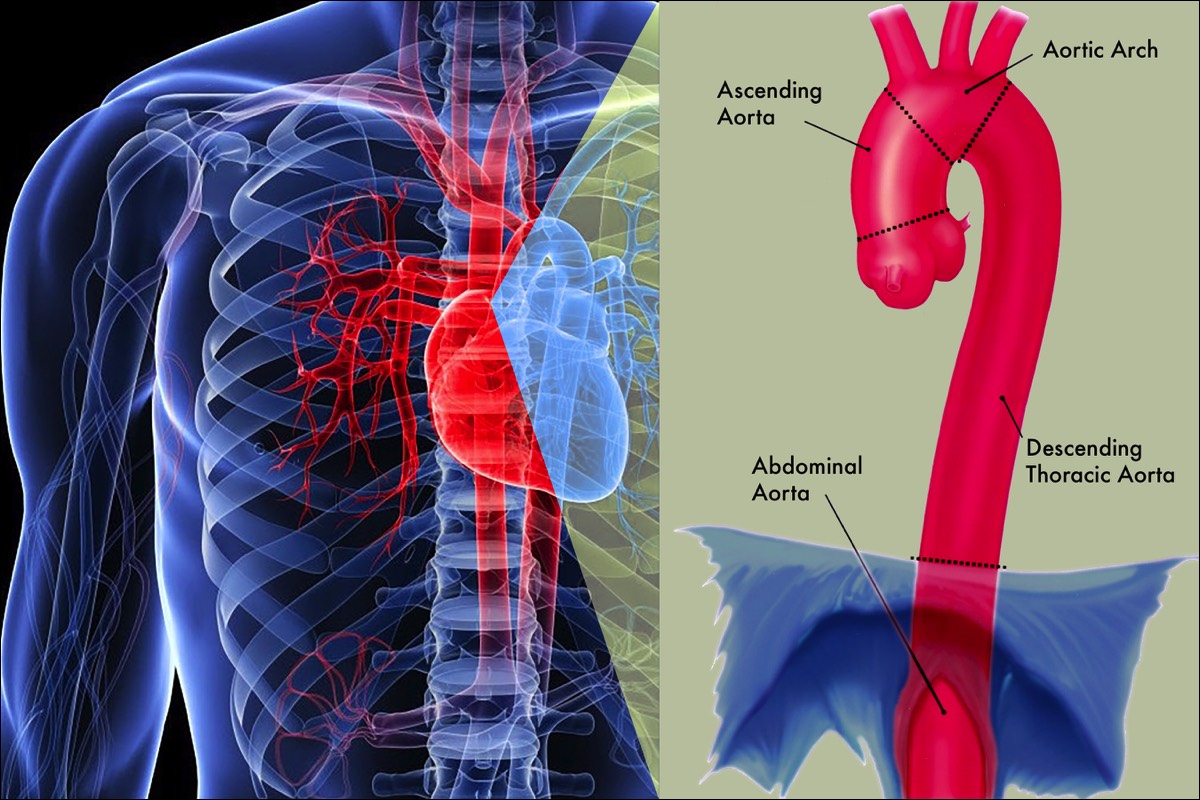
A thoracic aortic aneurysm, or TAA, is a widening or bulging of a section of the aorta within your chest, that slowly degenerates. The aorta, the body’s main blood vessel, starts at your heart, and extends all the way to your pelvis, where it branches toward your legs. The larger the aneurysm, the higher the risk it may rupture, leading to damage of the aortic wall and bleeding that could cause death. For this reason, it is crucial to seek early intervention.
The thoracic aorta is also prone to dissection, or a tearing of the wall of the aorta. When this occurs in the ascending aorta, or aortic arch, it represents a life-threatening emergency, which is typically treated with emergency surgery. When a dissection involves the descending thoracic aorta, emergency treatment is still required, but this rarely includes surgery.
Dissections of the descending aorta do weaken the wall of the aorta, and are prone to aneurysm formation.
A Healthy AortaThe aorta is divided into 4 sections: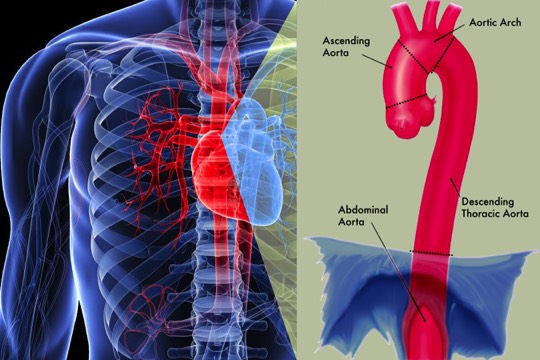
1) the ascending aorta
2) the aortic arch
3) the descending thoracic aorta
4) the abdominal aorta.
The section of the aorta that runs through the chest is called the thoracic aorta.
-
What are the Symptoms?
You may not feel any symptoms with TAA. Only half of patients with thoracic aortic aneurysms experience symptoms. Most TAA’s are detected when imaging studies are being done for an unrelated condition.
If you do have symptoms, they will depend on where your aneurysm is located and how large it is. Possible symptoms include:- Pain in the jaw, neck, and upper back
- Chest or back pain
- Coughing, hoarseness, or difficulty breathing
If your aneurysm is large and in the section of the aorta closest to the heart, it may affect your heart valves. This can result in shortness of breath or even heart failure if the leakage is severe.
Descending thoracic aneurysms are mostly asymptomatic, but they can occasionally cause back pain, and, if the aneurysm is large enough, it can cause abdominal pain. Most of the symptoms associated with stable thoracic aneurysms, are vague and non-specific. However, rupture or dissection of these aneurysms produce dramatic symptoms. Most patients report a ripping sensation in the chest, accompanied with severe pain in the back between the shoulder blades. Dizziness, fainting, difficulty walking and speaking can also accompany this acute event. This is a life-threatening situation and you should seek medical attention immediately. -
What are the Risk Factors?
It is not known why aortic aneurysms occur, but researchers understand some of the factors that contribute to their development. There certainly is a genetic component to many aneurysms that develop, and family members of people with aneurysms are at higher risk of developing one. Factors that may increase your risk for aneurysm formation include:
- Smoking
- High blood pressure
- Having a family history of aneurysms
- High cholesterol
- Genetic factors, such as an inherited weakness in the blood vessel wall, Marfan’s Syndrome, Ehlers-Danlos Syndrome, Loeys-Dietz Syndrome and Turner Syndrome.
- Injury
- Infection
-
How is a Diagnosis Made?
Our doctors will make a diagnosis based on your health history, physical exam, and certain tests, to help determine if you have a thoracic aortic aneurysm. Your physician will order a CTA (Computed Tomography Angiography). The scan will show the size of the aorta and exact location of the aneurysm.
What is a CTA?A CT (computed tomography) is a series of x-rays taken with a special machine. Computers use these x-rays to create three-dimensional images. CT angiography (CTA) combines a CT Scan with an injection of contrast fluid (dye) to produce pictures of blood vessels and tissues visible on the x-ray image.
Inform your doctor if you are allergic to the contrast fluid (dye) given during CTA scan. -
Treatment
Once your aneurysm is diagnosed, strict control of your blood pressure and the avoidance of smoking are two interventions which may prevent growth. There are currently no medications which can shrink an aneurysm or prevent it from growing.
If your TAA is small and not causing symptoms, your physician may recommend "watchful waiting,” which means that you will be monitored regularly for signs of changes in your aneurysm. Your physician may schedule you for a CTA scan every 6 months to a year, to watch the aneurysm. This test can help your physician monitor the size and shape of your aneurysm. This method is usually used for aneurysms that are smaller than about 2 inches across.
However, if your TAA is large or causing symptoms, you need active and prompt treatment to prevent rupture. Your vascular surgeon may recommend actively treating your aneurysm if it is large, grows quickly, or you have certain other types of disease. The active treatments for TAA are open surgical aneurysm repair and endovascular stent-graft repair.
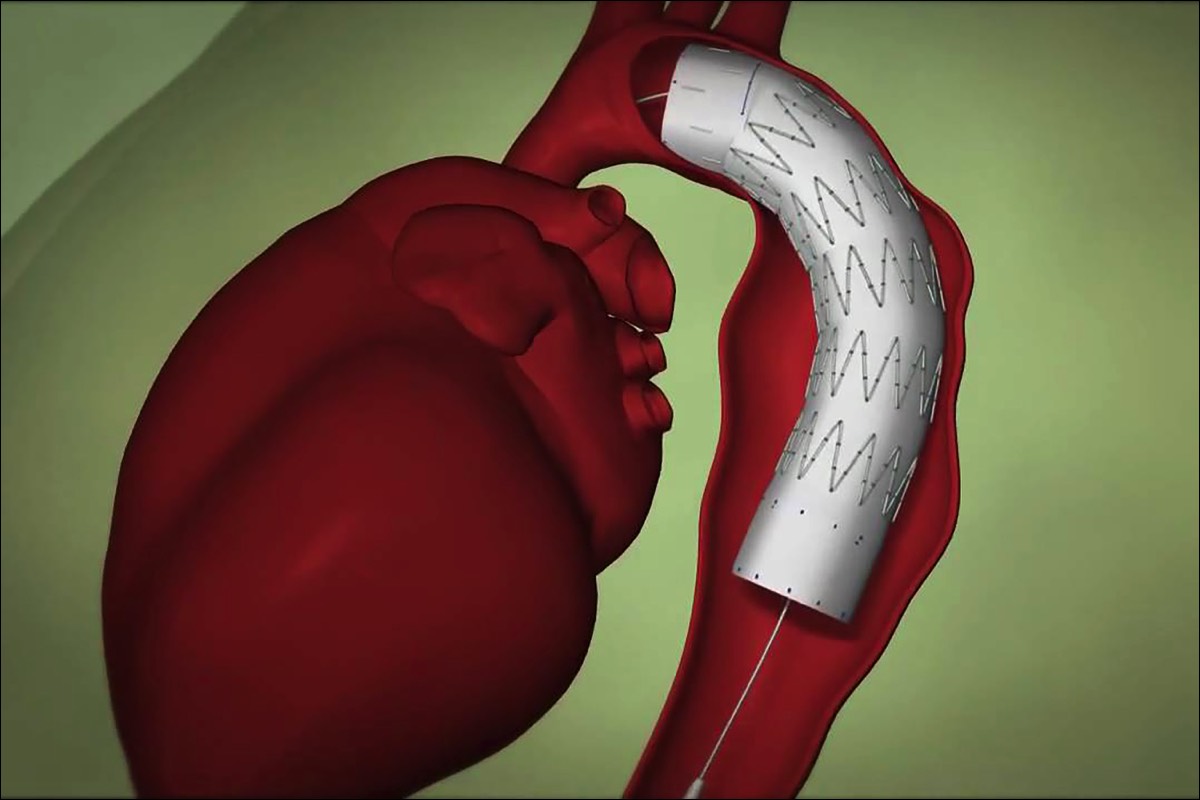
What is Open Surgical Repair?During open aneurysm repair, your surgeon makes an incision in your chest and replaces the weakened portion of your aorta with a fabric tube, called a graft. The graft is stronger than the weakened aorta and allows blood to pass through it without causing a bulge. Following the surgery, you may stay in the hospital for 7 to 10 days. If your aneurysm is extensive or complex, or if you have other conditions such as heart, lung or kidney disease, you may require 2 to 3 months for a complete recovery.
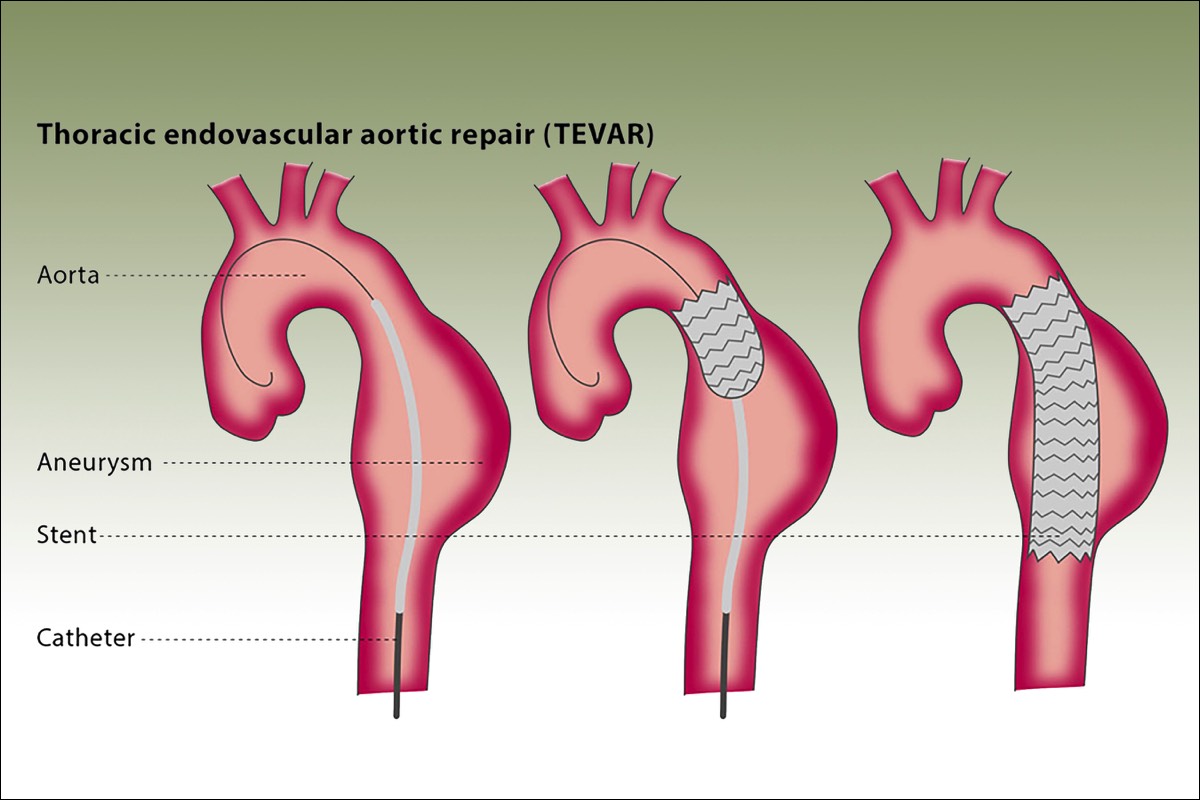
What is Endovascular Stent Graft Repair?Instead of open aneurysm repair, if your aneurysm location and shape is suitable, your vascular surgeon may consider a procedure called an endovascular stent graft. Endovascular means that the treatment is performed inside your body using long, thin tubes called catheters. The catheters are inserted in small incisions in your groin, and sometimes your arms, and are guided through your blood vessels. During the procedure, your surgeon will use live x-ray pictures viewed on a video screen to guide a stent-graft to the site of your aneurysm. Like the graft used in open surgery, this stent-graft allows blood to flow through your aorta without putting pressure on the damaged wall of your aneurysm. This keeps your aneurysm from rupturing. Over time, your aneurysm will usually shrink. Endovascular stent-graft repair is less painful, requires a shorter recovery time than open aneurysm repair, and your hospital stay is reduced to 2 or 3 days. However, this treatment may not be applicable to all TAAs, since your aneurysm must have a suitable shape to allow the stent-graft to be used effectively. With the endovascular stent-graft repair, it is particularly important that long-term follow-up with periodic scans of the aortic repair be done to be sure that the stent-graft is functioning properly. Sometimes further procedures are required to maintain the stent-graft if leaks develop or if it moves out of position.
Your vascular surgeon will advise you regarding the best option for your particular situation.Surgery Step 1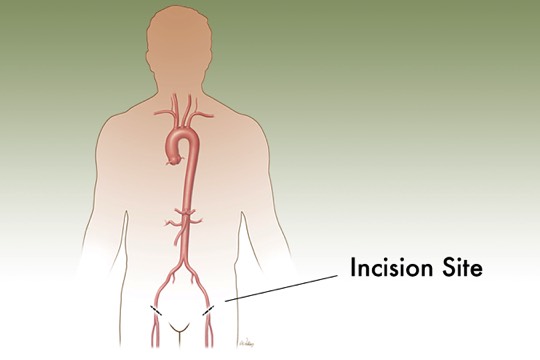 A small incision is made in the groin. A catheter is threaded through an artery. A collapsed stent-graft is placed inside the catheter.Surgery Step 2
A small incision is made in the groin. A catheter is threaded through an artery. A collapsed stent-graft is placed inside the catheter.Surgery Step 2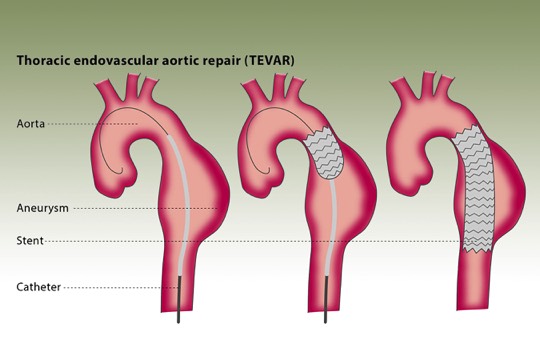 The surgeon uses x-ray guidance to move the graft through the arteries toward the damaged part of the aorta. The catheters are then used to place the graft in position.Surgery Step 3
The surgeon uses x-ray guidance to move the graft through the arteries toward the damaged part of the aorta. The catheters are then used to place the graft in position.Surgery Step 3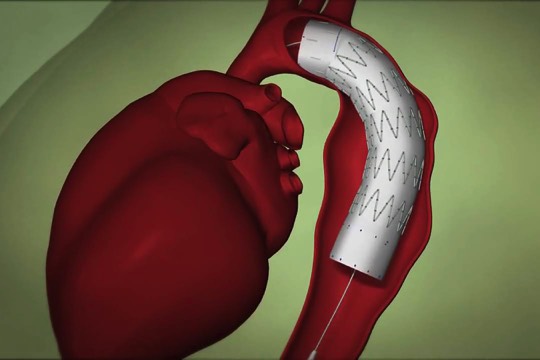 Once the stent-graft is in position, the surgeon expands it into the aorta. The catheters are then removed.
Once the stent-graft is in position, the surgeon expands it into the aorta. The catheters are then removed.
Endovascular Stent Graft Repair
-
After Treatment
If you've had open surgery, you can expect the cut (incision) in your chest to be sore for a few weeks. If you have stitches or staples in your incision, the doctor will take these out 1 to 3 weeks after surgery.
You will feel more tired than usual for several weeks after surgery. You may be able to do many of your usual activities after 4 to 6 weeks. But you will probably need 2 to 3 months to fully recover.
Keep all of your follow up doctor’s appointments.
Take your medication as directed.
After your procedure, you will have a follow up visit with your doctor within ten days. Your next appointment will be at one month, which will include a CT scan. You will have follow-up visits in 6 months, one year, and once a year every year after that.