-
Peripheral Arterial Disease / PAD
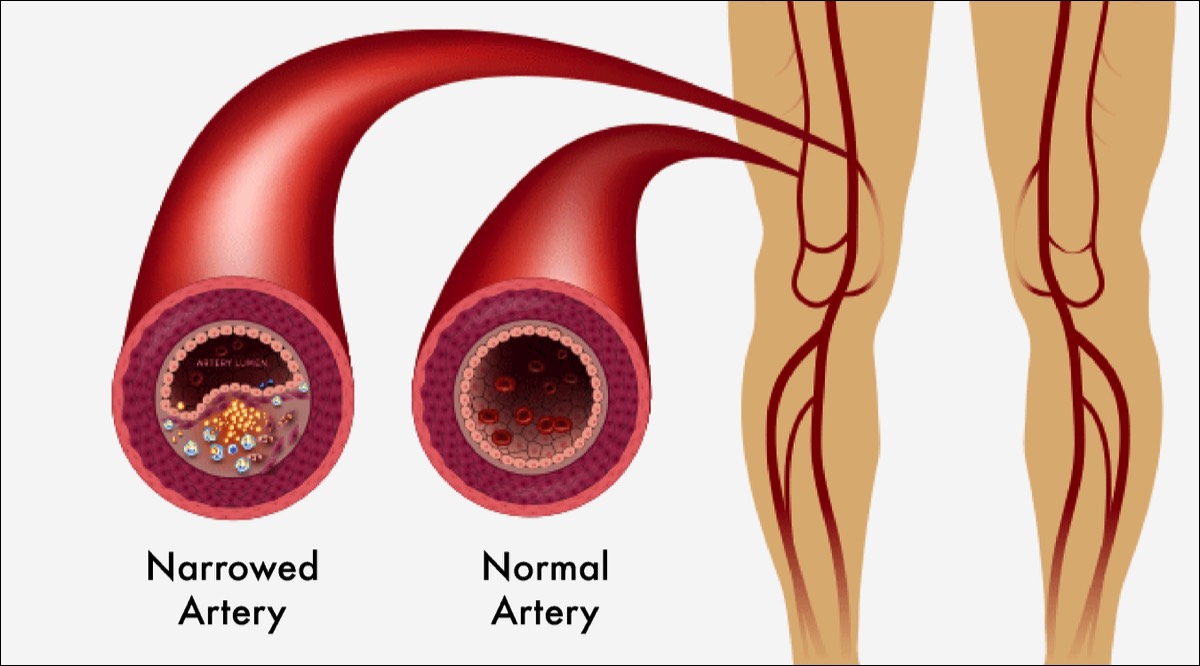
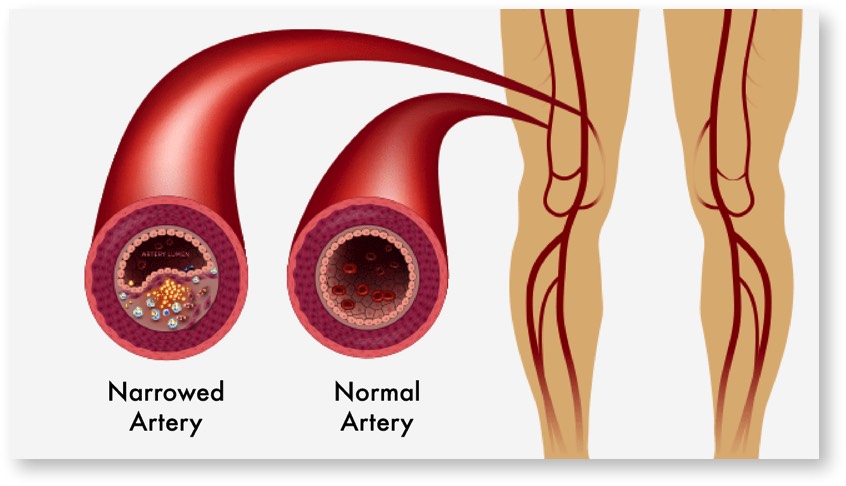
Peripheral Arterial Disease (PAD) is a chronic disease in which plaque builds up in the arteries to the legs. It affects 8.5 million people in the U.S., including 12-20% of people over the age of 60. This buildup typically occurs gradually. If allowed to progress, blood flow in that artery can become limited or blocked all together. This progressive disease can reduce the quality of life and mobility. Critical Limb Ischemia (CLI) is an advanced stage of PAD. This progressive condition occurs when there is significant blockage in the arteries, which reduces blood flow to areas such as the legs and feet. The lack of blood flow can lead to severe pain, even when at rest during the night, non-healing wounds below the ankle, gangrene and ultimately limb amputation. Without proper and immediate treatment, patients with CLI may risk amputation and related complications. Patients with PAD are also at risk for the development of stroke and heart attack.
 Unfortunately, PAD cannot be cured, but treatment along with healthy lifestyle choices, can improve blood flow, helping to keep the disease from getting worse.
Unfortunately, PAD cannot be cured, but treatment along with healthy lifestyle choices, can improve blood flow, helping to keep the disease from getting worse.
What Is PAD?
-
What are the Symptoms?
FATIGUE OR CRAMPING OF MUSCLES WHILE WALKING
Fatigue or cramping of your muscles (claudication) in the calf, thigh, hip, or buttock, may signal you have PAD. Typically, the discomfort is felt after walking a certain distance and goes away with rest. It’s likely to be worse when you climb stairs or go uphill.
PAIN IN TOES OR FEET WHILE RESTING
As PAD worsens, pain occurs at rest. If you have pain in your toes or feet while resting, you may have an advancing case of PAD.
OPEN WOUND ON TOES OR FEET
An open wound or ulcer on your toes or feet, often at a pressure point on the foot, can signal a serious case of PAD. An ulcer can progress to gangrene. These symptoms require immediate medical attention. -
What are the Risk Factors for PAD?
Certain health problems and habits increase the chances of developing PAD. The more risk factors you have, the greater your chances of getting PAD.
The most common risk factors include:- Smoking
- Diabetes
- Heart Disease, such as coronary artery disease
- Age: In the United States, people aged 50 and older have an increased risk for PAD
- High blood pressure
- High cholesterol, and a high fat diet
- High triglycerides
- Kidney failure
- Obesity
-
How is the Diagnosis Made?
Our doctors will make a diagnosis based on your health history, physical exam, and certain tests to help determine if you have PAD. Initial diagnostic tests for PAD, include an ankle-brachial index test and duplex ultrasound. Advanced testing include an angiogram to determine the extent of the disease and the treatment options.
What is an Ankle-Brachial Index Test?This is a common test used to diagnose PAD. It compares the blood pressure in your ankle with the blood pressure in your arm. To get a blood pressure reading, your doctor uses a regular blood pressure cuff and a special ultrasound device to evaluate blood pressure and flow.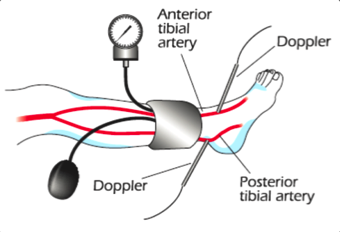
What is Duplex/Doppler Ultrasound?Ultrasound looks at the blood flowing through your arteries. Advanced imaging machines using ultrasound can painlessly and noninvasively produce pictures showing the blood vessels and the blood flowing through them. A small transducer is pressed against the skin utilizing sound waves to create images. A gel is applied to the skin to help the transducer create accurate images. The test can show changes in blood flow due to artery narrowing or blockage.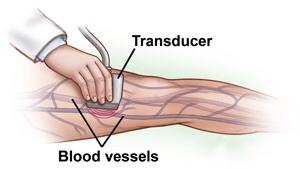
What is an Angiogram?An angiogram is an imaging test that uses x-rays and a special dye to see inside the arteries. It involves placing a thin tube into the artery and injecting dye into the arteries to see where the blockages are located.
Inform your doctor if you are allergic to the contrast fluid (dye) given during an angiogram. -
Treatment
PAD is usually treated by aggressively managing the risk factors with lifestyle changes and medication. This includes quitting smoking, controlling blood pressure and cholesterol, controlling diabetes, and losing weight. In addition, an exercise program, if followed faithfully, can significantly improve the symptoms of PAD in many cases.
If PAD is causing serious symptoms, further treatments such as balloon angioplasty, stent placement, atherectomy, or surgical bypass can be very effective in improving the blood flow to the affected leg.
Endovascular ProceduresFor a severely narrowed artery or a short blockage, endovascular procedures may be used. These can be done through a small incision rather than full incisions. As a result, recovery is often quicker and complications tend to be fewer. Endovascular procedures include angioplasty, and stenting. Both procedures use catheters (thin tubes) to reach blockages in your arteries.What is Angioplasty?Angioplasty is a procedure to open narrowed or blocked blood vessels that supply blood to your legs. Angioplasty uses a medical “balloon” delivered through a catheter, to widen blocked arteries. Once the artery is open, the balloon is deflated and removed. Oftentimes, a stent is placed at the same time the angioplasty is performed.Surgery Step 1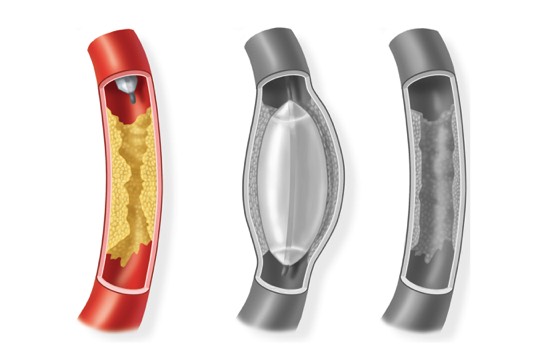 A balloon tipped catheter is inserted into the artery and threaded to the narrowing or blockage.Surgery Step 2
A balloon tipped catheter is inserted into the artery and threaded to the narrowing or blockage.Surgery Step 2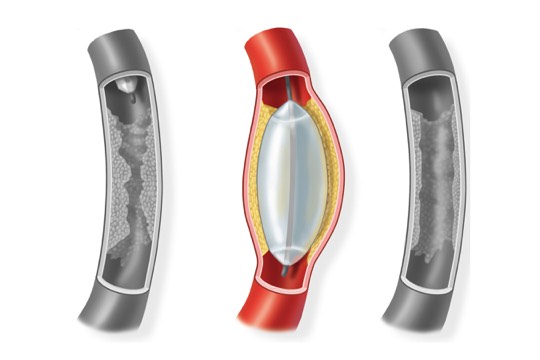 The balloon is inflated and deflated several times. This presses the plaque against the artery walls.Surgery Step 3
The balloon is inflated and deflated several times. This presses the plaque against the artery walls.Surgery Step 3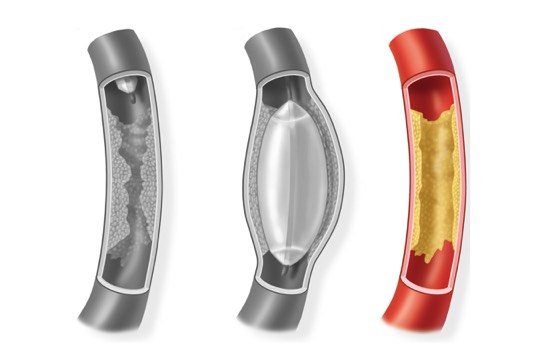 Once the artery is open, the balloon is deflated and removed. Blood flows freely through the widened channel.
Once the artery is open, the balloon is deflated and removed. Blood flows freely through the widened channel.
What is Angioplasty/Stent?Oftentimes after an angioplasty procedure, a stent, a tiny wire mesh device, is inserted into the artery to hold it open. Once it is placed, it remains in the artery.Surgery Step 1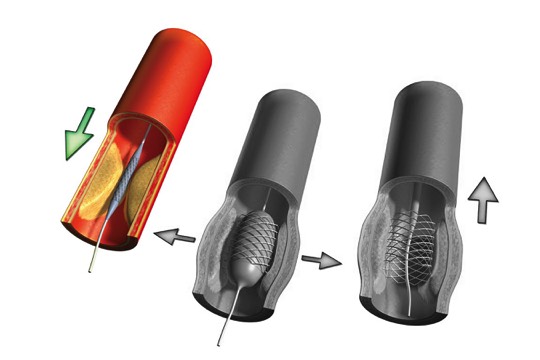 A collapsed stent is mounted onto a balloon catheter and guided across the blockage.Surgery Step 2
A collapsed stent is mounted onto a balloon catheter and guided across the blockage.Surgery Step 2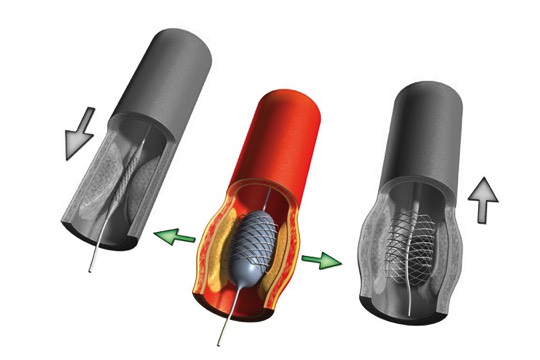 The balloon is inflated to open the stent, which locks into place inside the artery.Surgery Step 3
The balloon is inflated to open the stent, which locks into place inside the artery.Surgery Step 3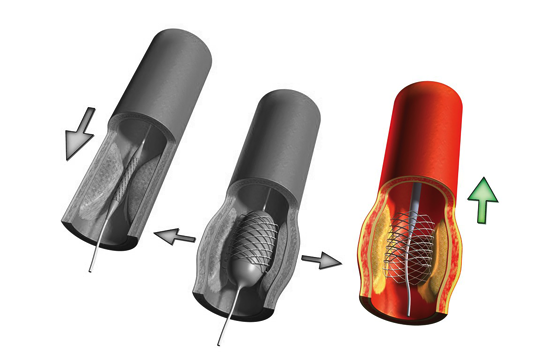 The balloon is deflated and removed. The stent remains in place, holding the artery open.
The balloon is deflated and removed. The stent remains in place, holding the artery open.
Angioplasty Stent
What is Atherectomy?
Atherectomy is a procedure that utilizes a catheter with a blade or rotary device on the end, to remove plaque from a blood vessel. Your surgeon will then scrape away the plaque with the catheter blade.©2019 Medtronic. All rights reserved.
Used with the permission of Medtronic.
Atherectomy Procedure
©2019 Medtronic. All rights reserved. Used with the permission of Medtronic.
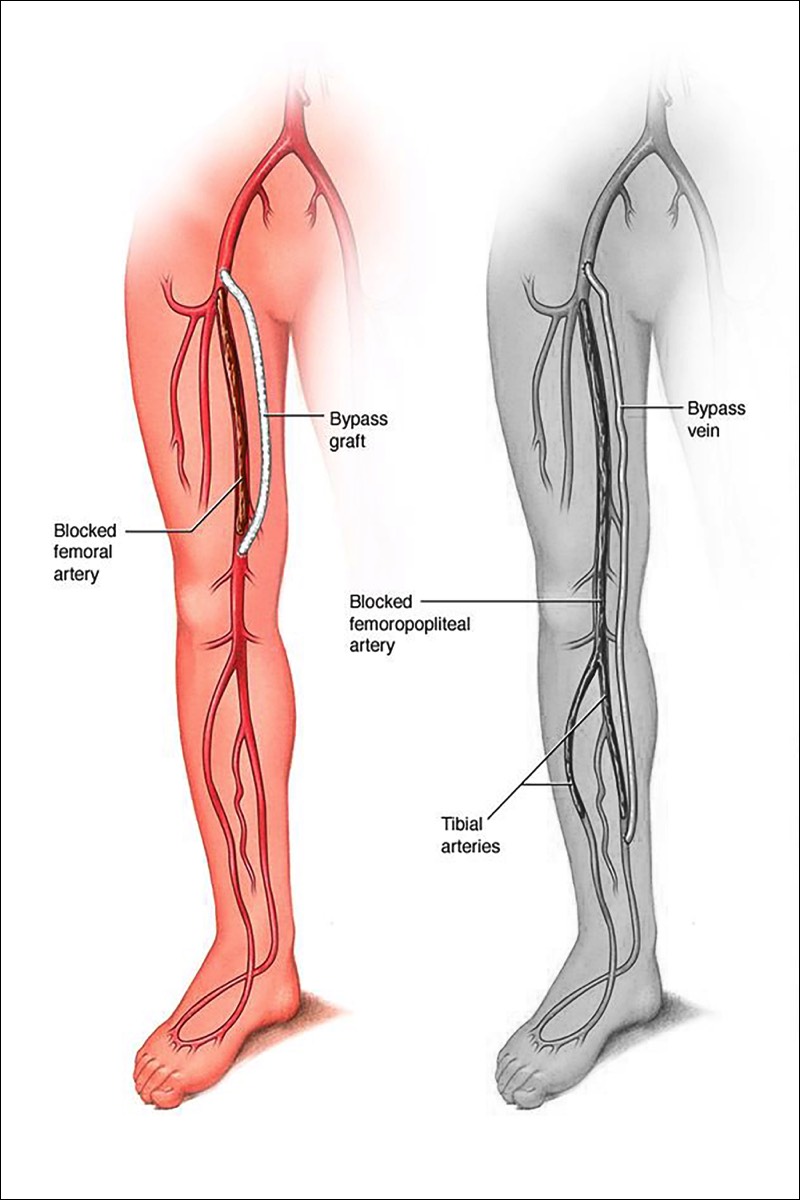
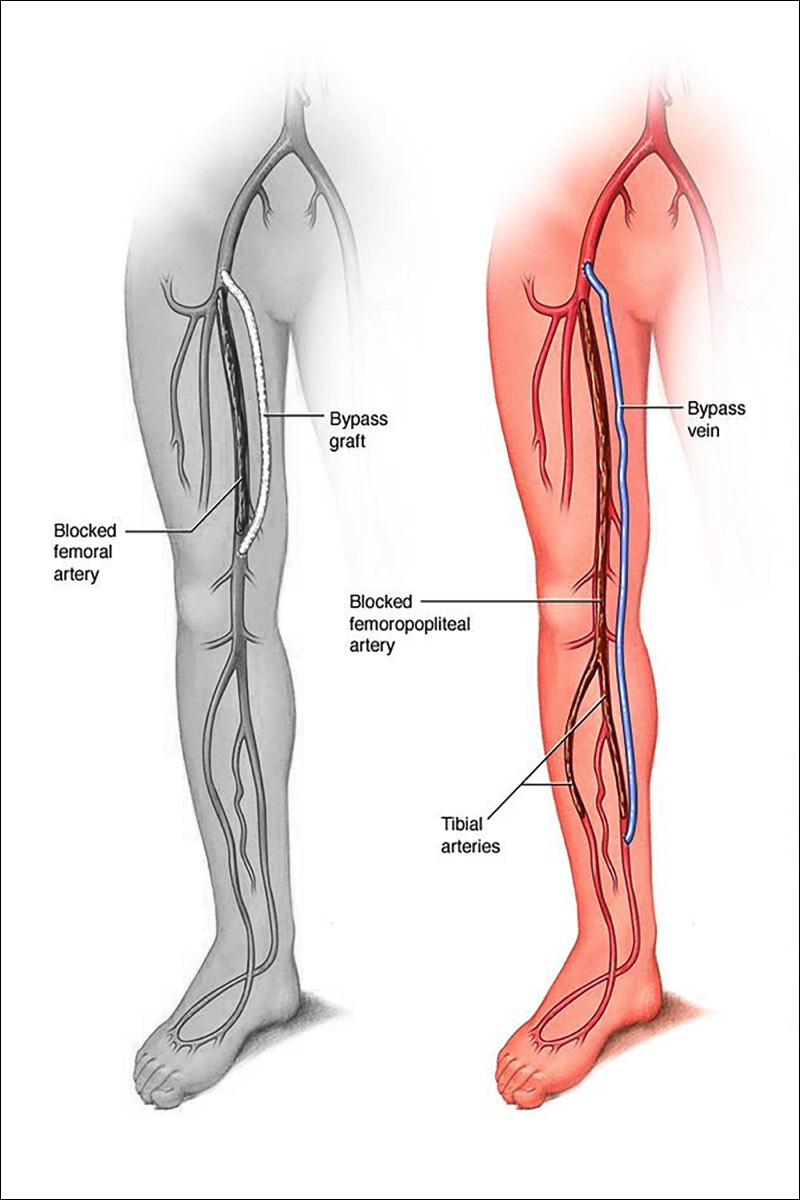
What is Bypass Surgery?Bypass is a surgical procedure that uses a special tube called a graft, to redirect blood flow around an area of blockage in the leg. The procedure creates an alternate channel for blood flow, bypassing an obstructed or damaged vessel. The graft may come from a healthy section of the patient's own vein, or a synthetic material. The graft is sutured to the artery above and below the blockage.
Types of Peripheral Bypass
Peripheral bypass grafts carry blood from the femoral artery in your thigh, to an artery further down your leg. There are two common types of peripheral bypasses. One type is used for the upper part of the leg, and the other type is used for the lower part of the leg. You will receive the type of bypass that fits your needs.Surgery Step 1Femoral - Popliteal Bypass - bypasses to the popliteal artery and ends behind the knee. Either your own vein or a synthetic material may be used for the graft.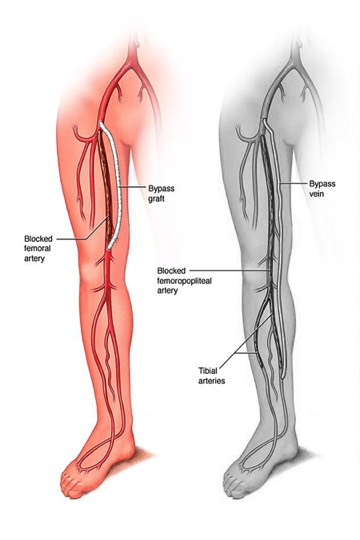 Surgery Step 2Femoral - Tibial Bypass - bypasses end below the knee. Either your own vein or a combined graft, made from your vein and a synthetic material, may be used.
Surgery Step 2Femoral - Tibial Bypass - bypasses end below the knee. Either your own vein or a combined graft, made from your vein and a synthetic material, may be used.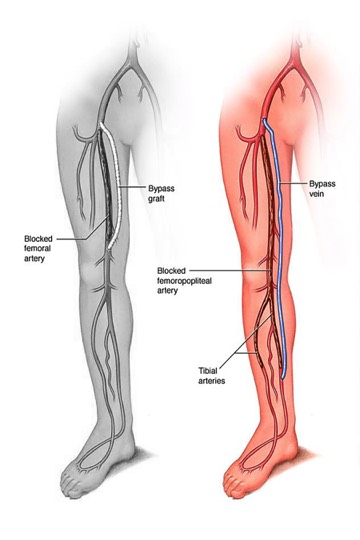
Types of Bypass GraftsA Blood Vessel Graft often comes from the same leg where you will have the bypass. These grafts are used on arteries above or below the knee. Grafts are removed and prepared at the time of the bypass. In some cases, a leg vein is left in place and connected to the artery (an in situ procedure). An angioscope (a thin tube with a camera attached) is used for an in situ procedure.Man-Made Grafts are synthetic grafts produced from materials that are easily accepted by the body. These grafts work best on arteries at or above the knee.
Right After Surgery
Following surgery, you will be monitored closely in the recovery room. From there, you may go to an intensive care unit, if needed. Once you are stable, you will be moved to a regular hospital room. Your leg may swell and be painful, but you may be given medication to control pain and prevent infection.
As You Regain Strength
You will start walking soon. Walking is an important part of your recovery. Walking reduces swelling and helps your incision heal. Walking also prevents lung problems, such as pneumonia. The sooner you recover in the hospital, the sooner you can go home. Wear slippers or shoes to protect your feet. Elevate your leg whenever you are sitting. Tell a nurse right away if you have chest pain, foot pain, or shortness of breath. Also let your surgeon know if your incision is draining or if you have constipation.
Recovering At Home
You can leave the hospital when your surgeon says it is OK. Be sure to have someone drive you. Expect to have some leg swelling after surgery. This will lessen over time.
No matter what procedure you have, these measures help your body heal more quickly:- Keep your appointments with your surgeon so they can check your leg.
- Take medications as directed.
- Care for incisions as instructed.
- Shower or take sponge baths. Don’t take a tub bath without your doctor’s okay. Avoid skin burns by testing the temperature of the water beforehand.
- Don’t stand or sit with your feet down for too long. When you sit, raise your foot as high as you comfortably are able by placing a pillow under your calf for support.
- Have staples or sutures removed when your doctor recommends.
- Drink plenty of fluids.
- Try to walk a little farther each day.
-
Living a Healthier Life
Maintaining a healthier lifestyle can help slow disease. It can also improve the overall health of your arteries, reducing the chance of a heart attack or stroke.
Exercise Daily
Frequent exercise is important for your health. Walking may improve your blood pressure and circulation. It helps your body develop many small artery branches (collateral arteries). These small arteries can improve blood flow around blockages. If you have diabetes, walking helps you control your blood sugar. To add walking to your day, follow these guidelines:- Start small. Walk to do errands close to your home.
- Walk on level ground, such as at a mall. Bring a friend or join a group to keep you going.
- Work up to walking for 30 minutes on most days.
Eat Healthy Foods
A healthy diet is a good way to lower your risk of PAD. It helps prevent plaque build-up and reduces blood pressure and cholesterol levels. For the greatest health benefits:- Eat at least 5 servings of fruits and vegetables each day. They contain fiber, vitamins, minerals, and antioxidants.
- Limit red meat, dairy products, and processed foods. Instead, choose chicken, fish, or tofu.
- Bake, broil, or steam foods. They taste great and have less fat.
- Follow diet changes that can help control health problems. Use less salt if you have high blood pressure. Limit sugar and carbohydrates if you have diabetes.
- Eat smaller portions to reach or maintain a healthy weight.
Stop Smoking
Each cigarette you smoke damages your arteries. Smoking also decreases circulation and makes a graft more likely to fail. These tips may help you quit smoking:- Cut down slowly on the number of cigarettes you smoke each day.
- Set a date to stop smoking.
- Ask your surgeon about stop-smoking aids. Or ask your local hospital about stop-smoking programs if you need help.
Take Care of Your Feet
Circulation problems can make feet tender and easier to bruise or infect. Take care of your feet. Be sure to:- Wash and dry your feet carefully.
- Protect your feet with slippers, socks, or shoes.
- Ask a healthcare provider to trim your toenails.
Control High Blood Pressure
High blood pressure can injure your arteries and your graft. You can control your blood pressure. Remember to:- Take your medication as directed.
- Have your blood pressure checked regularly.
- Exercise often and lose excess weight.
- Use less salt if you have high blood pressure.